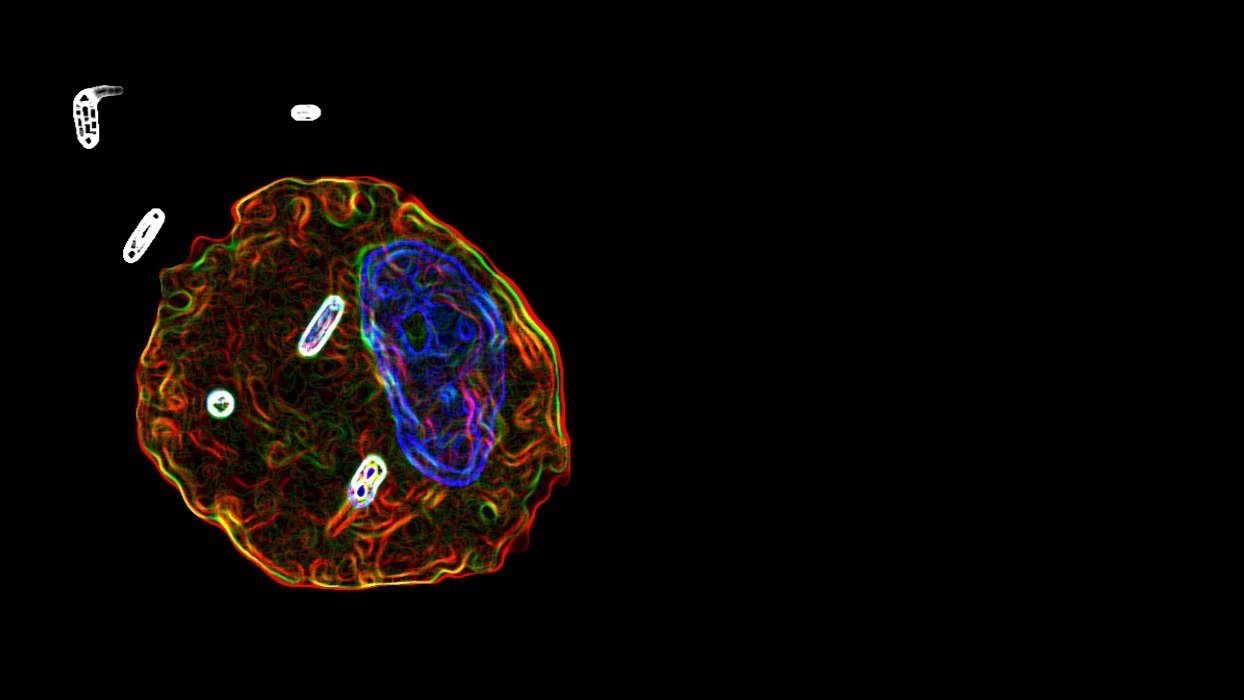
In the laboratory of Dr. Sebastián A. Riquelme, we study how metabolism regulates host-pathogen interaction. We are interested in learning how specific metabolic routes impact the function of both phagocytes and lymphocytes in response to airway pathogens during acute and chronic infection (immunometabolism). We focus on the mitochondrion, particularly in pathways used by this organelle to both generate energy and control inflammation. We have special curiosity for the pathology produced by the major human opportunists Pseudomonas aeruginosa and Staphylococcus aureus, which subsist in the respiratory tract via the production of biofilms. These biofilms evolve unique metabolic configurations to thrive, traits that are influenced by the immunometabolic activity of local inflammatory cells. Our approach involves in vitro and in vivo models of infection, as well as the analysis of samples from subjects colonized by P. aeruginosa and S. aureus, particularly individuals with cystic fibrosis (CF). Thus, our research is translational, using immunometabolism as platform to better comprehend how pathogens persist and induce inflammatory lung disease.
Bioenergetic Metabolism and Disease Tolerance During Pneumonia
Pulmonary pathogens, like P. aeruginosa and S. aureus, trigger a highly destructive inflammatory response to infection that compromises the ability of the host to breathe. To cope with this detrimental setting, the host is obligated to activate disease tolerance, which is an evolutionary conserved defense strategy that preserves tissue integrity by limiting damaging inflammation. However, how disease tolerance is established during bacterial pneumonia remains poorly understood. In our laboratory, we study how the host activates disease tolerance upon infection by either P. aeruginosa or S. aureus. More exactly, we are interested in dissecting how disease tolerance is regulated by both oxidative phosphorylation (OXPHOS) and glycolysis, the two major systems used by the host to produce energy. Using different in vivo models of pneumonia, we have found that the impact of these networks on disease tolerance is regulated by both ketogenesis and the immunoregulatory metabolite itaconate, which tune how pulmonary cells produce ATP and inflammatory mediators during infection. Currently, we are working on how P. aeruginosa and S. aureus sense and exploit this bioenergetic environment to exploit disease tolerance to coexist with their host (chronic infection).
Impact of nucleotide and nucleoside metabolism during pneumonia
The conservation of pulmonary homeostasis relies on the ability of airway cells to self-preserve. This process is highly regulated by the synthesis of nucleotides and nucleosides, which generate DNA, RNA, and many other signaling molecules that contribute to active tissue remodeling. However, how these pathways influence lung maintenance, pathogen survival, and inflammation during pneumonia remain unclear. Using P. aeruginosa and S. aureus as model opportunists, we study both in vivo and in vitro how different routes involved in the generation of nucleotides and nucleosides control infection and airway damage during pneumonia. We focus on the role of different ectonucleotidases, which control the manufacture of many anti-inflammatory nucleosides. Likewise, we are interested in the regulation exerted by the de novo pathway of pyrimidine synthesis, which associates with cell replication, mitochondrial energy production, and inflammation.
Cystic fibrosis, immunometabolism, and bacterial pathoadaptation
Cystic fibrosis (CF) is a genetic disease caused by mutations in the CF transmembrane conductance regulator (CFTR). A hallmark of CFTR dysfunction is the accumulation of a dense mucus layer in the airway of people with CF, which traps most inhaled opportunists. However, only a few of these organisms prevail, including P. aeruginosa and S. aureus, which readily adapt to this environment to chronically persist via the generation of biofilms. How these pathogens but not others thrive in this milieu remains poorly understood. We have found that both P. aeruginosa and S. aureus exploit specific metabolites produced by the mitochondria of host phagocytes to produce ATP and biofilms, such as succinate and itaconate. Currently, using in vitro and in vivo models of infection, as well as clinical samples, we are dissecting how novel immunometabolic circuits regulated by CFTR influence the bioenergetics and biofilms of both P. aeruginosa and S. aureus in the CF lung.